SEPA Patient Focus – Skin Cancer
PATIENT’S GUIDE TO SKIN CANCER
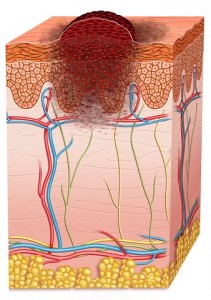
Skin cancer is the most common cancer in the United States. Nearly 50 percent of all cancers are skin cancers. Medical experts divide skin cancer into two groups: melanoma and non-melanoma. Non-melanoma is the most common type, but melanoma is deadlier, accounting for 75 percent of skin cancer deaths. The two main categories of non-melanoma skin cancer are basal cell and squamous cell carcinoma.
WHY IS SCREENING IMPORTANT FOR SKIN CANCER?
The earlier skin cancer is found, the better your chances are of being successfully treated. In fact, experts believe the cure rate for skin cancer could be 100 percent if all were brought to a physician’s attention before they had the chance to spread. The best tools for early detection are performing frequent self-examinations and communicating any suspected findings to your physician. Also, pay attention to comments from friends and family regarding changes in a mole or other mark on your skin.
WHAT CAN I DO TO DETECT SKIN CANCER EARLY
The best way to detect skin cancer is through monthly self-examinations of the skin, looking for new growths or changes to existing moles, freckles, or other marks. Use a full-length mirror for the exam. You may also wish to ask a family member to check hard-to-see areas, such as the scalp, the back, and the soles of the feet.
 WHAT ARE THE WARNING SIGNS OF SKIN CANCER
WHAT ARE THE WARNING SIGNS OF SKIN CANCER
Basal and squamous cell carcinoma are most commonly found on areas of the skin that receive the greatest amount of sun exposure—the head, face, neck, and arms. Warning signs that should be immediately discussed with your physician include:
- A wart-like growth with a rough surface that crusts or occasionally bleeds.
- A small, smooth, shiny pale or waxy lump that bleeds following minor injury. This lesion may be pink, white or yellow.
- A persistent scaly red patch with irregular borders that may crust or bleed.
- Open sores that bleed and crust and persist for weeks.
An elevated growth with a central depression that occasionally bleeds. This type of growth may rapidly increase in size and tiny blood vessels may appear on the surface.
Melanoma can occur on any skin surface. In men, lesions are most commonly found on the trunk (between the shoulders and the hips) or the head and neck. Women most commonly find their lesions on the lower legs. Use the warning signs below as a guide; however, some melanomas do not fit the pattern. If you are unsure if a mark is normal or not, ask your physician. If you notice any of the following warning signs, talk to your physician immediately:
- A new black, abnormal, or “ugly-looking” mole.
- Spots that change in size, shape, or color.
- One half of the mole’s shape doesn’t match the other half.
- The mole’s edges are ragged or notched with the pigment spreading into the skin.
- The mole’s color changes through the lesion. There may be shades of tan, brown, or black or patches of red, blue, or white.
- The mole is wider than 1/4 inch or an existing mole appears to be increasing in size (about the size of a pencil eraser head)
- A mole that was flat increases in height rapidly.
WHAT HAPPENS IF A SKIN CANCER IS SUSPECTED 
Not every mole or freckle is cancerous, but it’s important to have anything unusual checked by your doctor.
If you or your doctor finds a mark on your skin that is suspicious, you will have to have a biopsy to determine if you have skin cancer. There are several different kinds of skin biopsies, and your physician will determine what type you should have based on the size and location of the lesion. Possible biopsies include:
- “Shave” biopsy, where the skin is numbed and then the top layer of cells are “shaved” with a surgical blade.
- “Punch” biopsy, where the doctor numbs the skin and then uses a pen-sized “cookie cutter” type tool to cut through layers of skin for a cell sample.
- An “incisional” or “excisional” biopsy, where, after numbing, a wedge of skin is removed with a surgical knife. If the entire mole is removed, it is called an excisional biopsy.
After the cells are removed from your skin, a pathologist examines them under a microscope. The pathologist will look at the cells to see if any are cancerous. If they are, the pathologist will determine if the cancer is invasive or not and identify what kind of cancer is present.
In the pathology report, if the cells are cancerous, the pathologist often will give the biopsy a grade. In general, a lower grade number means a slower-growing cancer, while a higher number means a faster-growing cancer. The grade can help predict the patient’s prognosis — how successfully the skin cancer can be treated.
WHO IS AT RISK FOR SKIN CANCER?
The exact cause of skin cancer is not known, but certain risk factors are linked to the disease. The chance of getting skin cancer increases as you get older. Experts estimate that 40 to 50 percent of Americans who live to age 65 will develop skin cancer at least once
KNOWN RISKS FOR SKIN CANCER
- Fair skin: Caucasians are at a 20 times higher risk for skin cancer than African-Americans are. The risk is highest for people who freckle or burn easily, especially those with red or blond hair and blue or light-colored eyes.
- Exposure to ultraviolet (UV) radiation: The most common source of UV radiation is the sun. Tanning lamps also are a source of UV rays. People who live in geographic areas that receive more UV rays are at greater risk. For example, the risk is greater for those in the southern United States than in northern states like Minnesota and Maine.
- Family history: About 10 percent of people who develop melanoma have had a close relative with the disease.
- Weakened immune system: Individuals with weakened immune systems are at an increased risk for developing skin cancers, especially squamous cell carcinomas. This includes those people who have been treated with immune suppression medicines for organ transplants.
- Moles: Although moles are non-cancerous skin tumors, people with numerous moles and those who have abnormal or large moles are at an increased risk for melanoma.
HOW CAN I PREVENT SKIN CANCER?
- The best way to lower your risk for skin cancer is to be smart about sun exposure.
- Avoid the midday sun, and if you can’t stay inside use a sunscreen with a sun protection factor (SPF) of 15 or higher. This is necessary even on hazy days and in all four seasons. Sunscreen should be applied 30 minutes before expected exposure to the sun and reapplied every 2 hours and after swimming or excessive perspiration.
- Seek shade whenever possible.
- Wear a shirt and a wide brimmed hat to protect your body and wrap-around sunglasses with UV protection to protect your eyes.
- Avoid tanning beds or lamps.
Protect children and adolescents. Children who receive severe, blistering sunburns are at increased risk to develop melanoma later in life.
WHERE CAN I FIND MORE INFORMATION?
Click on image below to download your own printable copy of this handout